How Does Ebola Work?
The Hidden Role of Ebola in Immune Responses
An article published in 2018 by Younan, et al. titled “Disabling of lymphocyte immune response by Ebola virus,” draws to attention some interesting associations between lymphopenia, a significant reduction in T cells, and an Ebola virus infection. Most specifically, the author shows how the level of lymphopenia in a patient correlates to survival or fatality. Although the article lacks statistical findings and experimental data, it still provided relevant insight into some mechanisms behind Ebola infections, as well as future prospects in the area of therapeutics.
Introduction
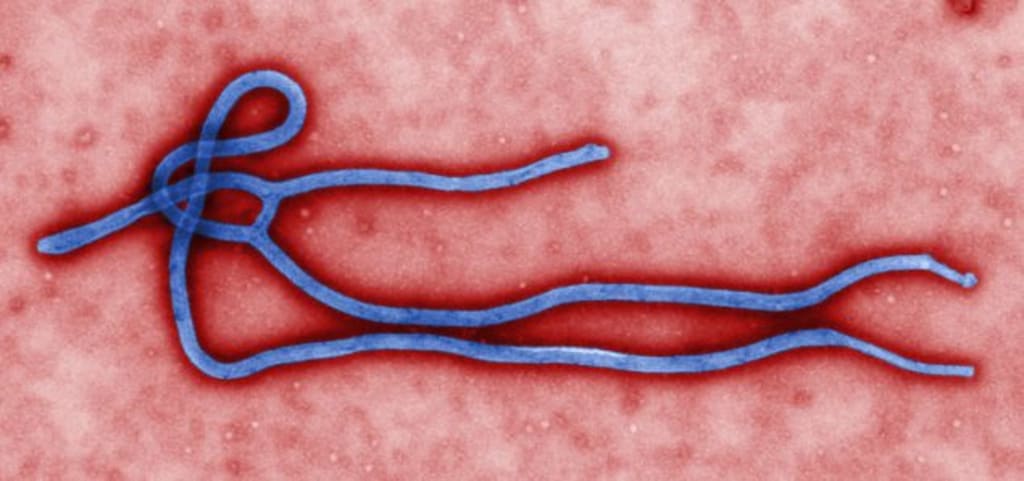
Since 2014, the Centers for Disease Control and Prevention has been working to contain the Ebola outbreak in West Africa. With numbers nearly equivalent to those presented by Younan and colleagues, the CDC puts total deaths as 11,325 as of April, 2016, making this the worst Ebola outbreak recorded in history. The term, Ebola virus (EBOV) most commonly refers to the species Zaire ebolavirus, one of five within the ebolavirus genus. EBOV’s are known to cause hemorrhagic fever in humans and mammals, often leading to death within six to sixteen days after symptoms arise. The EBOV consists of a negative-sense RNA genome that codes for one non-structural protein, and seven structural proteins, of which GP, VP35, and VP24 are of most important in Younan's research and will be discussed later.
Discussion
In their report, Younan and colleagues discuss the occurrence of lymphopenia in patients infected with the Ebola virus, stating that the virus depletes the body of cells critical to fighting the infection and important in the development of the adaptive immune system. Although providing no original or recent statistical data of their own, the authors linked higher T cell numbers throughout infection with survival and based on their citation, this data was determined through measurement of IgG (Immunoglobulin G) in survivors compared to the fatalities. Baize and colleagues, in 1999, found that the patients who succumbed to the infection had no IgG present as a result of lack of development of the adaptive immune response, as opposed to the survivors who had rising IgG levels throughout infection.
Partially to blame for the T cell death is the induction of a “cytokine storm” during an Ebola infection. This is due to an increase in viral replication in cells such as macrophages and monocytes, and a dramatic release of inflammatory mediators occurs. These include coagulation factors, free radicals, and anti- and pro-inflammatory cytokines. This “cytokine storm” is toxic to cells and leads to apoptosis of T cells, as well and tissue and organ damage ultimately resulting in a decrease in peripheral blood lymphocytes. One of the cytokines involved with inflammation, TNF-alpha, has been shown to be associated with necrotic cell death and apoptosis. Younan, et al. gives mention to TRAIL, TNF- related apoptosis inducing ligand, and its increase in expression in macrophages and monocytes during an infection. This is based off the data by Hensley and colleagues, whose methods utilized immunohistochemistry and RNA analysis to look for TRAIL expression in human monocytes/macrophages that were infected with EBOV.
During the outbreak in West Africa, there seemed to be reduced inflammatory responses seen in survivors as opposed to the documented fatalities. Based off of this data, it seemed that an individual’s outcome can be enhanced by the administration of immunosuppressive agents. In particular, the article speaks of Eritoran, a TLR-4 antagonist. Eritoran was initially being investigated for its use in sepsis but it failed to perform as hoped. However, researchers discovered that it seemed to be effective in controlling cytokine storm, which is a large contributor of T cell death seen in EBOV. According to the authors previous research regarding Eritoran, it was reported that the drug helps protect from the lethality of the Ebola virus, as well as in other associated viruses such as Marburg virus. Administration of Eritoran was shown to reduce signs of the disease, decrease viral titers, and reduce the severity of cytokine storm. The drug proved successful in decreasing the inflammatory response without reducing innate and adaptive immunity. Ultimately, treatment of EBOV requires the innate and adaptive arms of the immune system to remain intact, while suppressing the pro-inflammatory aspect.
Another treatment target exists where the EBOV virions interact with T lymphocytes. Activation of CD4 T cells requires interactions with both TLR-4 and GP on the viral envelope. The over expression of GP allows for “steric shielding” which impairs antigen presentation thus preventing T cell activation. The EBOV GP is bulky and prevents the interaction between the T cell and the MHC peptide. The 2014 outbreak was the first time the Zmapp cocktail was used. This cocktail includes monoclonal antibodies that are designed to target the bulky GP using mechanisms that are still not fully understood.
More recent studies have looked into the EBOV proteins VP35 and VP24, which are known to contain regions called “IIDs” (IFN- inhibiting domains). The effects of these domains lead to inhibition of signal transduction after TCR stimulation. The impaired downstream signaling is due to a lack of induction of the phosphorylation of adaptor molecules such as Zap70. The cause of this was found to be due to compromised dendritic cell maturation resulting from the IID’s in VP35 and VP24. Along with the effects of IID’s as seen in dendritic cells, similar effects are also seen in natural killer, and B cells. These IID’s disrupt adaptive immunity and promote lymphopenia, but when the virus is mutated, disabling VP35 IID, the effects are reversed and cell activation increases.
Conclusion
It is clear, from the work done by Younan and colleagues both past and present, that we are now able to target some of the unique features of EBOV virions to help aid in the survival of infected individuals. Much work has been done to formulate cocktails such as Zmapp, and more research is needed to open the door for even more effective therapies in the future. Studies need to be continued regarding the roles of IIDs and to help understand their importance in cell mediated responses. Now that we can see the clear link between fatalities and lymphopenia, our job is to dig deeper into understanding how the virus induces lymphocyte death, and how we can prevent it to aid in survival.






Comments
There are no comments for this story
Be the first to respond and start the conversation.